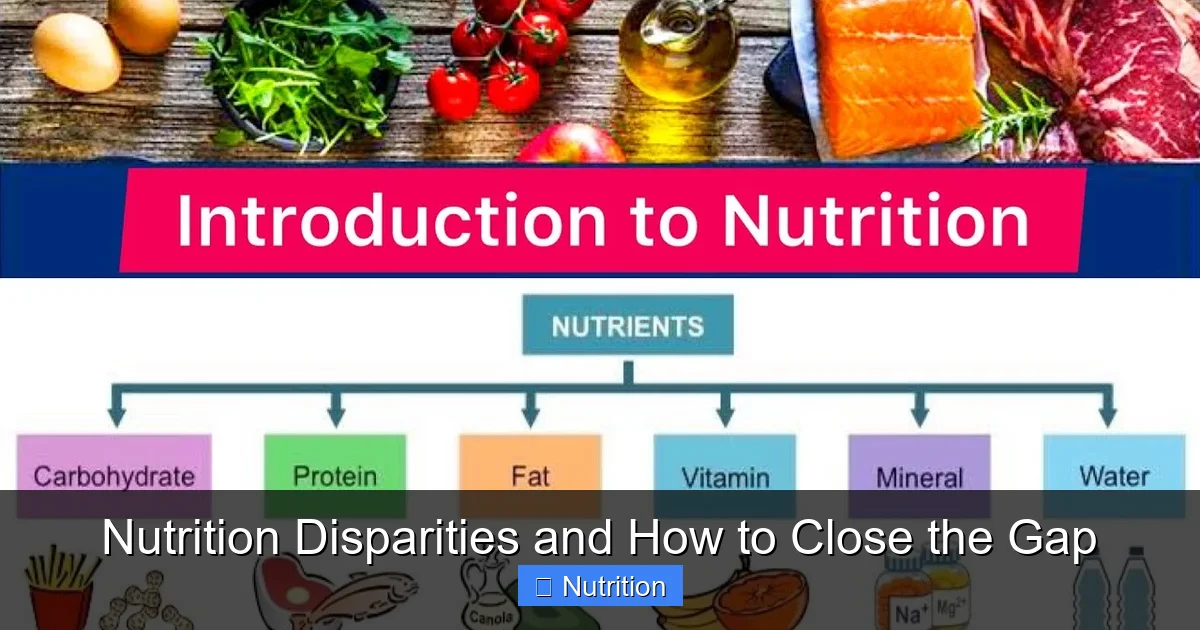
Featured image for this comprehensive guide about nutrition in rural areas
Image source: i.ytimg.com
The gentle sway of wheat fields under an endless sky, the quiet hum of a tractor, the close-knit warmth of a small town – these are the idyllic images often conjured when we think of rural America. Yet, beneath this picturesque facade, a silent crisis is unfolding, impacting the health and well-being of millions. This crisis is rooted in profound nutrition disparities in rural areas, a systemic challenge that limits access to affordable, healthy food and, in turn, fuels a host of preventable health issues.
Far from urban centers overflowing with supermarkets and diverse dining options, rural communities often find themselves navigating a complex landscape of limited choices. Distances are greater, incomes are often lower, and the infrastructure to support a robust, healthy food system can be sparse. These factors combine to create significant barriers to optimal nutrition in rural areas, leaving many residents vulnerable to diet-related diseases and chronic health conditions that could otherwise be avoided.
Understanding the intricacies of these disparities is the first step toward building a healthier future for rural populations. This comprehensive guide will delve into the root causes, explore the far-reaching health consequences, and, most importantly, highlight innovative and actionable strategies being implemented to close the gap and ensure that every individual, regardless of their zip code, has the opportunity to thrive through good nutrition.
Quick Answers to Common Questions
What’s the biggest challenge when it comes to nutrition in rural areas?
The primary hurdle is often limited access to fresh, affordable, and nutritious food due to fewer grocery stores, long distances, and inadequate transportation options for residents.
Why is healthy eating so difficult to achieve for families in these regions?
Beyond access, factors like lower income levels, a lack of nutrition education, and the higher cost of healthy options contribute to the struggle for good nutrition in rural areas, making convenient, less healthy choices more common.
Who is most affected by poor nutrition in rural areas?
Vulnerable populations, including children, the elderly, and low-income families, often bear the brunt, facing higher risks of diet-related health issues due to these persistent food disparities.
What are some quick ways communities can start to improve nutrition in rural areas?
Initiatives like setting up community gardens, supporting local food pantries, establishing mobile markets, and advocating for local food systems can make a tangible difference by bringing fresh produce closer to home.
Can education play a significant role in boosting rural nutrition?
Absolutely! Providing practical nutrition education workshops, cooking classes, and resources on healthy food preparation can empower individuals and families to make better dietary choices, even with limited resources, enhancing overall nutrition in rural areas.
📋 Table of Contents
- The Silent Crisis: Understanding Rural Nutrition Disparities
- Root Causes: Why Healthy Food Access is a Challenge in Rural Areas
- The Health Impact: Consequences of Poor Rural Nutrition
- Data Snapshot: Illuminating Rural Nutrition Challenges
- Innovative Solutions: Bridging the Rural Food Gap
- Collaborative Pathways: Building Sustainable Rural Nutrition Systems
- Conclusion: Cultivating a Healthier Future for Rural America
The Silent Crisis: Understanding Rural Nutrition Disparities
When we talk about nutrition disparities in rural areas, we’re not just discussing a lack of food; we’re talking about a lack of access to nutritious food. While food insecurity exists everywhere, it often manifests differently and with greater severity in non-urban settings. Rural residents frequently face what are commonly known as “food deserts” – geographic areas where access to affordable, healthy food options, like fresh fruits, vegetables, and whole grains, is severely limited or non-existent. Instead, these areas might be dominated by “food swamps” – an abundance of convenience stores, fast-food outlets, and gas stations primarily offering highly processed, calorie-dense, and nutrient-poor options.
Learn more about nutrition in rural areas – Nutrition Disparities and How to Close the Gap
Image source: wembrace.in
According to the U.S. Department of Agriculture (USDA), millions of Americans live in low-income areas with low access to grocery stores. A significant portion of these areas are rural. This lack of access isn’t just an inconvenience; it’s a fundamental determinant of health. Without ready access to fresh produce, lean proteins, and whole grains, diets often become reliant on less healthy, shelf-stable, and often cheaper alternatives. This dietary pattern contributes significantly to the prevalence of obesity, diabetes, and heart disease that disproportionately affects rural populations. Addressing nutrition in rural areas requires a nuanced understanding of these unique challenges.
| Nutritional Indicator | Rural Area Prevalence/Data | Urban Area Prevalence/Data | Primary Contributing Factor(s) |
|---|---|---|---|
| Child Stunting (Under 5 years) | 25-35% | 10-20% | Limited access to diverse food, poor sanitation, inadequate health services. |
| Anemia in Women (15-49 years) | 40-55% | 25-40% | Iron-poor diets, high disease burden, limited prenatal care, heavy physical labor. |
| Severe Food Insecurity (Households) | 15-25% | 5-10% | Poverty, reliance on subsistence farming, limited market access, climate shocks. |
| Access to Diversified Diets | Lower access to nutrient-rich foods (e.g., fruits, vegetables, animal products) | Higher access to varied markets and processed foods (quality varies) | Limited market infrastructure, low income, insufficient dietary knowledge. |
| Access to Essential Nutrition Services | Limited or no access to specialized nutrition programs, health facilities, or fortified foods. | Generally better access to health clinics, public health initiatives, and diverse food options. | Geographic isolation, lack of trained personnel, weak infrastructure, transport barriers. |
What Defines “Nutritional Disparity”?
- Limited Access: Not enough grocery stores selling fresh produce, meat, and dairy within a reasonable distance.
- Affordability: Even if fresh options exist, they may be priced higher due to transportation costs, making them inaccessible for low-income families.
- Quality and Variety: Fewer options for diverse, culturally appropriate, and high-quality foods compared to urban supermarkets.
- Transportation Barriers: Lack of personal vehicles or public transportation to reach distant food sources.
- Knowledge Gaps: Limited access to nutrition education and cooking skills resources.
These combined factors create a challenging environment where making healthy choices becomes an uphill battle, often contributing to the higher rates of food insecurity and poor dietary quality observed in many rural communities. The goal of closing rural nutrition disparities is not just about bringing in more food, but about creating sustainable systems where healthy food is readily available, affordable, and culturally appropriate for everyone.
Root Causes: Why Healthy Food Access is a Challenge in Rural Areas
The web of factors contributing to inadequate nutrition in rural areas is complex and interconnected. It’s not a single problem but a confluence of geographic, economic, social, and infrastructural barriers that collectively make healthy food access a significant hurdle for rural residents. Understanding these root causes is essential for developing effective and sustainable solutions to tackle rural nutrition disparities.
Learn more about nutrition in rural areas – Nutrition Disparities and How to Close the Gap
Image source: asja.org
Geographic Isolation and Infrastructure
One of the most immediate and obvious challenges in rural settings is sheer distance. Many rural communities are characterized by vast expanses between population centers and vital services, including grocery stores. The absence of robust public transportation systems means that residents without personal vehicles are often stranded, unable to reach the nearest supermarket, which might be tens of miles away. Poor road conditions or seasonal weather can further exacerbate these transportation challenges, making even a short trip daunting. This isolation dramatically limits choices, often forcing reliance on the nearest, albeit unhealthy, options.
Economic Barriers
Economic realities play a crucial role in shaping rural nutrition. Rural areas often face lower median incomes and higher poverty rates compared to urban areas. This financial strain means that even if nutritious food is available, it might be unaffordable. Furthermore, the cost of living, particularly transportation expenses (like gas for long drives to the store), can eat into already tight budgets, leaving less disposable income for food. The limited presence of major employers also means fewer jobs with competitive wages and benefits, perpetuating a cycle of economic hardship that directly impacts food security and dietary quality. Federal nutrition assistance programs like SNAP and WIC, while vital, can also be challenging to utilize if there are no participating retailers within a practical distance.
Limited Retail Landscape (“Food Deserts” and “Food Swamps”)
The supermarket landscape in rural areas has dwindled over decades. As large chain stores consolidate, they often close smaller, less profitable branches in rural towns, leaving behind a void. What remains are often smaller convenience stores, dollar stores, or gas stations, which typically stock a limited selection of highly processed, shelf-stable, and often more expensive items, with little to no fresh produce. This phenomenon, often termed a “food desert,” is further compounded by “food swamps,” where unhealthy food options overwhelm the environment. The lack of competition also means that the few existing stores may have less incentive to offer diverse, high-quality products, further exacerbating the challenge of maintaining good nutrition in rural areas.
Healthcare Access and Education
Beyond direct food access, the support systems for healthy eating are also scarce in rural regions. There are fewer healthcare providers, including registered dietitians and nutritionists, meaning residents have limited access to professional guidance on healthy eating, disease management through diet, or cooking skills. Educational initiatives around nutrition are often underfunded or simply non-existent. While telehealth has grown, persistent gaps in broadband internet access in many rural areas can make even virtual nutrition counseling difficult. This lack of educational resources and professional support can leave individuals without the knowledge and tools needed to navigate complex food choices and prepare healthy meals, even if ingredients become available.
The Health Impact: Consequences of Poor Rural Nutrition
The pervasive challenges to achieving optimal nutrition in rural areas are not abstract problems; they translate directly into tangible and severe health consequences for millions. The chronic lack of access to healthy, affordable food and supporting nutrition education contributes significantly to a higher burden of diet-related diseases, impacting individuals, families, and the overall vitality of rural communities. Addressing rural nutrition disparities is, therefore, a critical public health imperative.
Chronic Disease Burden
Perhaps the most significant impact of poor rural nutrition is the disproportionately high rates of chronic diseases observed in these populations. Rural adults and children often experience higher rates of obesity, type 2 diabetes, cardiovascular disease (including hypertension and heart disease), and certain types of cancer compared to their urban counterparts. These conditions are directly linked to diets high in processed foods, unhealthy fats, sugars, and low in fruits, vegetables, and whole grains. The challenge is compounded by limited access to preventative care, regular screenings, and ongoing disease management resources, turning treatable conditions into life-long struggles that diminish quality of life and place immense strain on healthcare systems.
Maternal and Child Health
The impact of inadequate nutrition in rural areas begins even before birth. Pregnant women in rural settings may struggle to access the nutrient-rich foods essential for healthy fetal development, leading to increased risks of adverse birth outcomes, including low birth weight and premature birth. For children, poor nutrition in early life can have long-lasting effects on cognitive development, academic performance, and overall physical health. Childhood obesity rates are often higher in rural areas, predisposing children to early onset of diabetes, heart disease, and other chronic conditions, setting them on a trajectory of lifelong health challenges.
Mental Health and Well-being
The connection between diet and mental health is increasingly recognized. Diets rich in processed foods and sugars can negatively impact mood, increase inflammation, and contribute to mental health issues like depression and anxiety. For individuals in rural areas already facing social isolation, economic stress, and limited access to mental health services, poor nutrition can exacerbate these challenges. Furthermore, the chronic stress of food insecurity itself – the constant worry about where the next meal will come from – can take a significant toll on mental well-being, creating a vicious cycle where stress impacts eating habits, which in turn impacts mental health.
Economic Productivity and Community Vitality
Beyond individual health, the consequences of poor rural nutrition ripple throughout the entire community. A population struggling with chronic illness due to poor diet is less productive in the workforce, leading to decreased economic output and higher healthcare costs. Children with nutrition-related health issues or food insecurity often perform poorly in school, limiting their future opportunities and the long-term potential of the community. Ultimately, persistent rural nutrition disparities can undermine the social fabric and economic vitality of rural towns, hindering their ability to thrive and attract new residents or businesses.
Data Snapshot: Illuminating Rural Nutrition Challenges
To truly grasp the scope of nutrition disparities in rural areas, it’s helpful to look at some illustrative data. While specific numbers can vary by region and study, consistent trends emerge when comparing health and food access indicators between rural and urban populations. These figures underscore the urgency of addressing nutrition in rural areas and highlight where interventions are most needed.
The table below provides a general overview of common disparities. These figures represent approximate ranges often reported by various health and agricultural agencies, reflecting the systemic nature of these challenges.
| Indicator | Rural Areas (Approximate) | Urban Areas (Approximate) | Source/Context |
|---|---|---|---|
| Adult Obesity Rate | 35-40% | 28-32% | Consistently higher in many rural counties (CDC, USDA) |
| Diabetes Prevalence | 13-15% | 10-12% | Often linked to diet and healthcare access (CDC) |
| Households with Limited Supermarket Access | Up to 20% | 5-10% | USDA Economic Research Service data on food deserts |
| Food Insecurity Rate | 12-14% | 10-12% | Slightly but consistently higher in rural areas (USDA) |
| Access to RDs/Nutritionists per 100k people | Significantly lower (e.g., <5) | Higher (e.g., 15+) | Reflects overall rural healthcare workforce shortages |
| Consumption of Fruits & Vegetables (daily servings) | Lower than recommended (e.g., 2-3) | Closer to recommended (e.g., 3-4) | General dietary intake studies |
This snapshot clearly illustrates a pattern: rural areas consistently lag behind their urban counterparts in key health and food access metrics. These disparities are not accidental; they are the result of deeply embedded systemic issues that require targeted and comprehensive interventions. The goal of mitigating rural nutrition disparities involves a multifaceted approach that addresses these underlying indicators and improves the overall landscape of nutrition in rural areas.
Innovative Solutions: Bridging the Rural Food Gap
The challenges of nutrition in rural areas are significant, but they are not insurmountable. Across the country, communities, non-profits, and government agencies are developing and implementing innovative solutions to bridge the rural food gap and foster healthier eating habits. These initiatives demonstrate that with creativity, collaboration, and commitment, it is possible to make meaningful progress in addressing rural nutrition disparities.
Expanding Food Access Points
One of the most direct ways to combat limited access is to bring healthy food closer to where people live. This involves a variety of strategies:
- Mobile Food Markets and Pantries: Vehicles equipped to carry fresh produce and other healthy staples can travel to underserved rural communities on a regular schedule, acting as rolling grocery stores or food banks.
- Farmers’ Markets and CSAs (Community-Supported Agriculture): Supporting local farmers’ markets and ensuring they accept SNAP/WIC benefits can provide direct access to fresh, local produce. CSAs allow consumers to buy a share of a farm’s harvest, receiving regular boxes of seasonal produce.
- Rural Grocery Store Initiatives: Programs that provide technical assistance, financing, or incentives to help establish new community-owned grocery stores (co-ops) or revitalize existing independent rural stores.
- Online Grocery and Delivery Services: Expanding online grocery delivery options to rural zip codes, combined with programs that subsidize delivery fees for low-income households, can bring supermarkets to residents’ doorsteps.
Leveraging Technology and Telehealth
Technology offers powerful tools for overcoming geographic barriers, though reliable internet access remains a prerequisite:
- Tele-nutrition Services: Remote dietary counseling, virtual cooking classes, and online support groups led by registered dietitians can provide crucial education and personalized guidance to rural residents who cannot easily access in-person services.
- Nutrition Apps and Digital Resources: Developing user-friendly apps that help with meal planning, healthy recipe ideas, grocery budgeting, and local food resource navigation can empower individuals to make healthier choices.
- Broadband Expansion: Investing in robust broadband infrastructure in rural areas is fundamental to leveraging any digital health or food access solution.
Promoting Nutrition Education and Skills
Access to food is only part of the equation; knowing what to do with it is equally vital:
- Hands-on Cooking Classes: Offering practical, culturally appropriate cooking classes that focus on preparing healthy meals with readily available ingredients can boost confidence and culinary skills.
- Community and School Gardens: Establishing community gardens not only provides fresh produce but also serves as an educational tool, teaching gardening skills and fostering a connection to food sources. School gardens can integrate nutrition education into the curriculum.
- Budgeting for Healthy Food: Workshops that teach strategies for maximizing federal nutrition benefits (SNAP, WIC) and making healthy food choices on a limited budget can be incredibly impactful.
These diverse approaches, when integrated and tailored to specific community needs, hold the key to building more resilient and healthier food systems in rural America, fundamentally transforming nutrition in rural areas.
Collaborative Pathways: Building Sustainable Rural Nutrition Systems
Tackling nutrition disparities in rural areas requires more than just individual programs; it demands a systemic, collaborative approach. Sustainable solutions emerge when various stakeholders – government, non-profits, local businesses, healthcare providers, and community members – work in concert to create environments where healthy choices are the default, not the exception. Building robust and equitable food systems is key to improving nutrition in rural areas for the long term.
Policy Interventions and Government Support
Government policies at local, state, and federal levels play a pivotal role in shaping food access and health outcomes:
- Strengthening Federal Nutrition Programs: Expanding and streamlining programs like SNAP (Supplemental Nutrition Assistance Program) and WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) to ensure they are easily accessible and provide adequate support for purchasing nutritious foods.
- Healthy Food Financing Initiatives (HFFI): Providing grants, loans, and tax credits to incentivize grocery stores and healthy food retailers to establish or expand in underserved rural communities.
- Transportation Subsidies: Funding programs that offer vouchers or support for public or ride-share transportation to grocery stores in rural areas.
- Zoning and Land Use Policies: Encouraging local governments to adopt zoning policies that facilitate the establishment of grocery stores and restrict the proliferation of unhealthy fast-food outlets in proximity to schools and residential areas.
Community-Driven Initiatives
The most effective solutions often originate from within the communities themselves, leveraging local knowledge and assets:
- Local Food Policy Councils: Bringing together farmers, community leaders, consumers, and public health officials to identify local food system challenges and develop tailored solutions.
- Partnerships Between Farms, Schools, Hospitals, and Food Banks: Creating networks where local farms supply fresh produce to schools (Farm-to-School), hospitals (Farm-to-Hospital), and food banks, thereby boosting local economies and improving community nutrition.
- Volunteer Networks: Organizing volunteers for food distribution, community garden maintenance, or assisting seniors and individuals with disabilities in accessing groceries.
- Culturally Appropriate Food Programs: Ensuring that food assistance and educational programs respect and incorporate the diverse cultural food preferences of rural populations, which increases engagement and effectiveness.
Empowering Local Agriculture
Supporting local food producers is a win-win: it strengthens rural economies and provides fresh, healthy food closer to home:
- Support for Small and Mid-sized Farms: Providing resources, training, and market access for smaller farms to help them thrive and supply local markets.
- Food Hubs: Establishing regional food hubs that aggregate, store, process, and distribute food from multiple local farms to various institutional and retail buyers, streamlining the supply chain for healthy food.
- Promoting Regenerative Agriculture: Encouraging farming practices that enhance soil health, biodiversity, and ecosystem services, leading to more resilient local food systems.
- Direct-to-Consumer Models: Facilitating direct sales channels like farm stands, U-pick operations, and online farmers’ markets that directly connect consumers with local produce.
These collaborative pathways represent a holistic approach to transforming nutrition in rural areas. By fostering strong partnerships and implementing supportive policies, we can build sustainable food systems that ensure equitable access to healthy food, closing the significant gap of rural nutrition disparities and fostering thriving rural communities.
Conclusion: Cultivating a Healthier Future for Rural America
The journey to address nutrition disparities in rural areas is multifaceted and complex, reflecting generations of disinvestment and systemic challenges. We’ve explored how geographic isolation, economic hardships, limited retail landscapes, and a scarcity of nutrition education converge to create significant barriers to healthy eating. The consequences are profound, manifesting as higher rates of chronic diseases, compromised maternal and child health, and an overall diminishment of community vitality. The data clearly underscores that nutrition in rural areas is not just an individual challenge but a critical public health and economic issue requiring urgent attention.
Yet, the narrative is far from one of despair. Across rural America, innovative solutions are taking root, demonstrating the power of community resilience and strategic intervention. From mobile food markets and tele-nutrition services to robust policy changes and empowered local agriculture, the pathways to a healthier future are emerging. These efforts, though varied, share a common thread: the recognition that solving rural nutrition disparities requires a collaborative spirit, an understanding of local needs, and a commitment to long-term sustainability.
Closing the gap in nutrition in rural areas is not merely about providing more food; it’s about building equitable food systems, fostering economic opportunity, enhancing education, and strengthening the social fabric of our rural communities. It demands a collective effort from policymakers, healthcare providers, local leaders, farmers, and every individual who believes in the right to health and well-being, regardless of where they call home. By working together, we can cultivate a future where every rural community thrives, nourished by accessible, affordable, and wholesome food, ensuring that the picturesque beauty of rural life is matched by the vibrant health of its people.
Frequently Asked Questions
What are the key challenges regarding nutrition in rural areas?
Rural areas often face significant hurdles to achieving optimal nutrition, primarily due to limited access to affordable, fresh, and healthy food options. This is often exacerbated by longer distances to grocery stores, fewer transportation options, and a prevalence of convenience stores lacking diverse produce.
Why do rural communities often experience greater nutrition disparities?
Nutrition disparities in rural areas stem from a combination of factors including lower median incomes, limited job opportunities, and a lack of infrastructure for food distribution. These socio-economic challenges make it difficult for residents to afford or access nutritious foods regularly.
What are the health consequences of poor nutrition in rural populations?
Poor nutrition in rural populations contributes to higher rates of chronic diseases such as type 2 diabetes, heart disease, and obesity. Children in these areas may also experience developmental delays and academic struggles due to inadequate diets, impacting long-term health and well-being.
What strategies can help improve nutrition in rural areas and close the gap?
Improving nutrition in rural areas requires multi-faceted approaches, including supporting local food systems like farmers’ markets, establishing community gardens, and improving transportation access to grocery stores. Policy changes that incentivize healthy food retailers and expand nutrition assistance programs are also crucial.
Are there successful programs or initiatives specifically designed to enhance nutrition in rural areas?
Yes, many initiatives are working to improve nutrition in rural areas, such as mobile food markets that bring fresh produce to remote communities and federal programs like SNAP and WIC, tailored to increase food access. Community-led efforts focusing on food literacy and cooking skills also play a vital role.
How can individuals and local communities contribute to better nutrition outcomes in rural settings?
Individuals can advocate for local food policy changes, volunteer at food banks or community gardens, and support local farmers. Communities can organize food cooperatives, establish educational workshops on healthy eating, and explore partnerships to bring fresh food resources closer to residents, fostering improved nutrition.


