Featured image for this comprehensive guide about depression symptoms
Image source: frontiersin.org
Common Depression Symptoms and Treatment Options
In a world that often demands constant positivity and resilience, it can be incredibly challenging to admit when you’re struggling. Yet, beneath the surface for millions, lies a profound and persistent emotional battle known as depression. It’s more than just a passing feeling of sadness; it’s a complex mental health condition that can profoundly impact every aspect of an individual’s life, from their thoughts and feelings to their physical well-being and daily functioning. Recognizing the common depression symptoms is the crucial first step toward healing and recovery.
If you or someone you know has been feeling “off” for an extended period, experiencing a persistent low mood, or noticing significant changes in behavior, it’s vital to understand what might be happening. Depression is a real medical illness, not a sign of weakness, and it affects people from all walks of life, regardless of age, gender, or background. According to the World Health Organization (WHO), more than 280 million people worldwide suffer from depression, making it one of the leading causes of disability globally. This blog post aims to shed light on the diverse symptoms of depression, provide actionable insights, and guide you towards understanding the various treatment options available.
Navigating the complexities of mental health can feel overwhelming, but remember: you are not alone. By equipping yourself with knowledge about depression symptoms, you empower yourself to seek help, support loved ones, and foster a path towards improved mental well-being. Let’s delve into the signs and signals that often indicate a struggle with depression, moving past the misconception that it’s merely a temporary blue mood.
Quick Answers to Common Questions
What are the main signs of depression symptoms?
Beyond just feeling sad, common **depression symptoms** include a persistent low mood, loss of interest in activities you once enjoyed, and significant changes in sleep or appetite. You might also feel constantly tired or struggle with concentration.
Is feeling sad always a symptom of depression?
While sadness is a core component, not all sadness indicates depression. **Depression symptoms** are characterized by sadness that is intense, persistent (lasting at least two weeks), and significantly impacts your daily life, often accompanied by other changes.
Can depression symptoms affect my physical health too?
Absolutely! Many people experience physical **depression symptoms** like chronic fatigue, unexplained aches and pains, headaches, or digestive issues. These physical sensations are just as real as emotional ones and shouldn’t be ignored.
How long do these depression symptoms usually last before it’s a concern?
If you’re experiencing several **depression symptoms** consistently for two weeks or more, it’s generally considered a significant concern. This persistent duration is a key indicator that it might be more than just a passing “funk.”
When should I seek help for depression symptoms?
It’s always a good idea to seek help if your **depression symptoms** are making it difficult to function, causing significant distress, or if you’re worried about them. Don’t wait until things become unbearable; early intervention can make a big difference.
📋 Table of Contents
- Understanding Depression: More Than Just Sadness
- The Emotional Landscape: Core Psychological Symptoms of Depression
- Beyond the Mind: Physical and Behavioral Symptoms of Depression
- Recognizing the Red Flags: When to Seek Professional Help for Depression Symptoms
- Navigating the Path to Recovery: Effective Treatment Options for Depression
- Living Well with Depression: Long-Term Management and Support
- Conclusion: Taking the First Step Towards Hope and Healing
Understanding Depression: More Than Just Sadness
Before we dive into the specific depression symptoms, it’s important to differentiate clinical depression (also known as major depressive disorder) from everyday sadness or grief. While sadness is a normal human emotion that everyone experiences, especially in response to loss or disappointment, depression is a persistent, pervasive condition that significantly interferes with daily life for weeks, months, or even years. It’s a mood disorder characterized by a sustained low mood and/or loss of pleasure or interest in activities, alongside several other criteria.

Learn more about depression symptoms – Common Depression Symptoms and Treatment Options
Image source: res.cloudinary.com
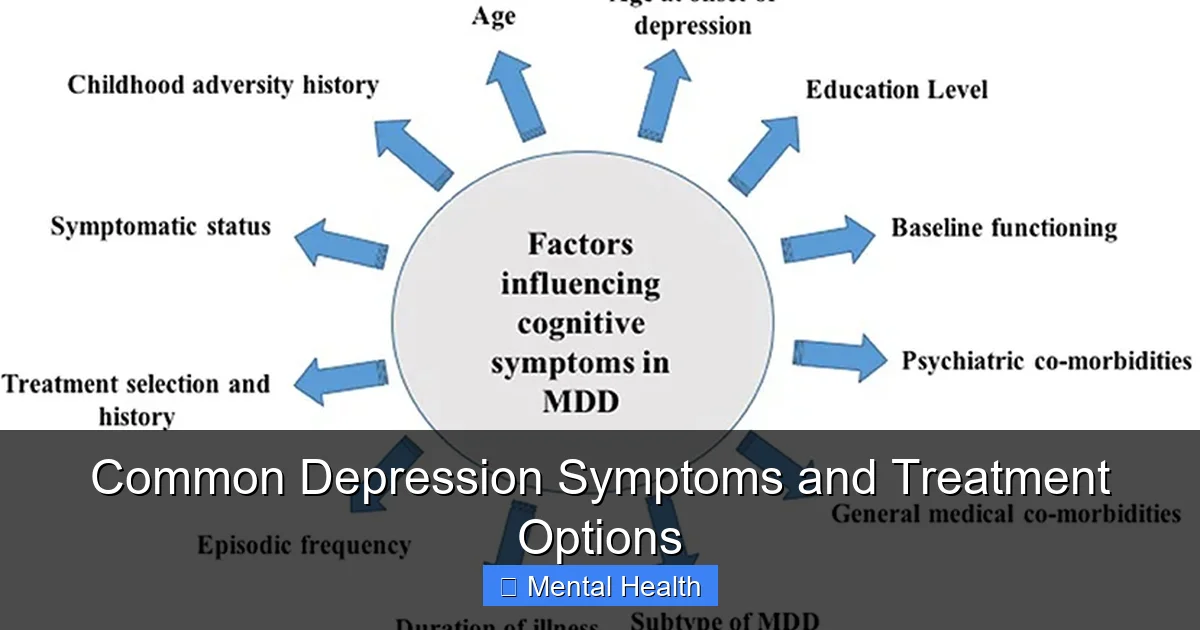
The experience of depression is highly individual. What one person feels may differ from another, but there are underlying commonalities that mental health professionals look for. These signs of depression aren’t always obvious; they can manifest subtly and gradually, making them difficult to pinpoint initially. Understanding that depression involves changes in brain chemistry, genetics, life events, and even physical health can help destigmatize the condition and encourage a more compassionate approach to oneself and others. Recognizing these complex factors is key to truly understanding common depression symptoms.
| Symptom Category | Key Symptom Description | Clinical Note / Impact |
|---|---|---|
| Emotional / Mood | Persistent Sadness, Emptiness, or Irritability | A core diagnostic criterion; must be present most of the day, nearly every day, for at least two weeks. Affects approximately 280 million people globally. |
| Behavioral / Motivational | Loss of Interest or Pleasure (Anhedonia) | Another core diagnostic criterion; inability to enjoy activities once found pleasurable. One of two “major” symptoms required for diagnosis. |
| Physical / Somatic | Significant Sleep Disturbances (Insomnia or Hypersomnia) | Can manifest as difficulty falling/staying asleep or sleeping too much. Affects over 80% of individuals with depression. |
| Cognitive | Difficulty Thinking, Concentrating, or Making Decisions | Often described as “brain fog.” Can significantly impair daily functioning, academic performance, and work productivity. |
| Energy / Vitality | Fatigue and Loss of Energy | Feeling tired all the time, even after adequate rest. This symptom is reported by nearly all individuals with major depressive disorder. |
Types of Depression to Be Aware Of
While this post focuses on general depression symptoms, it’s worth noting there are different types, each with unique characteristics and specific diagnostic criteria:
- Major Depressive Disorder (MDD): The most commonly recognized form, characterized by severe symptoms of depression that interfere with your ability to work, sleep, study, eat, and enjoy life. These episodes typically last for at least two weeks.
- Persistent Depressive Disorder (PDD) / Dysthymia: A chronic form of depression where symptoms may be less severe than MDD but last for at least two years (one year for children and adolescents). Individuals with PDD may also experience episodes of major depression.
- Seasonal Affective Disorder (SAD): Depression with a seasonal pattern, typically occurring during autumn and winter months due to reduced sunlight exposure. It often remits in spring and summer.
- Postpartum Depression (PPD): A more severe, long-lasting form of “baby blues” experienced by some women after childbirth. PPD can impact a mother’s ability to care for herself and her baby.
- Bipolar Disorder: While distinct from unipolar depression, it involves mood swings cycling between periods of depression and periods of mania or hypomania (elevated or irritable mood, increased energy). It’s crucial to differentiate these, as treatment approaches differ significantly.
Recognizing the nuances between these conditions is best done by a professional, but being aware of their existence can help you frame your own experiences and discussions with a healthcare provider about your depression symptoms.
The Emotional Landscape: Core Psychological Symptoms of Depression
The heart of depression often lies in its profound impact on one’s emotional and cognitive state. These are the common depression symptoms that people most readily associate with the condition. They can be debilitating, making even the simplest tasks feel insurmountable and clouding one’s perception of the world. Understanding these emotional shifts is paramount to identifying and addressing the condition effectively.
Learn more about depression symptoms – Common Depression Symptoms and Treatment Options
Image source: frontiersin.org
Persistent Sadness, Emptiness, or Irritability
This is perhaps the most well-known of the depression symptoms. A pervasive feeling of sadness, hopelessness, or emptiness that doesn’t lift, even when circumstances improve. It’s not just a momentary low; it’s a deep-seated despair that colors everything. For some, especially adolescents and young adults, depression may manifest more as persistent irritability, frustration, or anger rather than overt sadness. This constant state of negativity can be exhausting and make it difficult to connect with others, leading to further isolation.
Loss of Interest or Pleasure (Anhedonia)
One of the hallmark signs of depression is anhedonia – the inability to feel pleasure or interest in activities once enjoyed. Hobbies that used to bring immense joy, social outings, sexual activity, or even everyday activities like eating a favorite meal now feel dull, meaningless, or simply too much effort. This profound loss of zest for life can lead to further withdrawal and isolation, perpetuating the depressive cycle and making it harder to engage in beneficial activities.
Feelings of Worthlessness, Guilt, or Hopelessness
Many individuals experiencing depression symptoms struggle with intense feelings of worthlessness, self-blame, or excessive guilt, often disproportionate to actual events. They might ruminate on past mistakes, feel like a burden to others, or believe they are fundamentally flawed and undeserving of happiness. This negative self-talk erodes self-esteem and can make it difficult to accept support or see a way out of their situation, fostering a deep sense of hopelessness about the future.
Difficulty Concentrating, Remembering, or Making Decisions
Cognitive impairment is a significant, yet often overlooked, aspect of depression symptoms. People might find it hard to focus at work or school, follow conversations, read a book, or make even minor decisions. Their mind feels foggy, and their memory may seem less sharp. This “brain fog” can contribute to feelings of inadequacy, reduce productivity, and further impact daily functioning, making it challenging to maintain responsibilities.
Recurrent Thoughts of Death or Suicide
This is perhaps the most serious and alarming of all depression symptoms and requires immediate attention. Thoughts about death, dying, self-harm, or suicide are serious indicators of severe depression. These thoughts are not a sign of wanting to die, but often a desperate desire to escape overwhelming emotional pain and distress. If you or someone you know is experiencing these thoughts, please seek help immediately. You are not alone, and there are resources available, such as the National Suicide Prevention Lifeline (call or text 988 in the US) or emergency services (911). Reaching out is a sign of immense strength.
Beyond the Mind: Physical and Behavioral Symptoms of Depression
While depression is primarily a mental health condition, its impact extends far beyond the mind, manifesting in various physical and behavioral ways. These often subtle depression symptoms can sometimes be the first indicators that something is amiss, yet they are frequently misinterpreted or dismissed as unrelated issues. Recognizing these somatic and behavioral changes is critical for a holistic understanding of depression.
Changes in Sleep Patterns
Sleep disturbances are incredibly common symptoms of depression, and they can significantly impact an individual’s energy and mood. This can manifest in several ways:
- Insomnia: Difficulty falling asleep, staying asleep (waking up frequently during the night), or waking up too early in the morning and being unable to return to sleep. This type of sleep deprivation can worsen depressive feelings.
- Hypersomnia: Excessive sleeping, often feeling unrefreshed even after long hours of sleep. This isn’t just about feeling tired; it’s a persistent, overwhelming urge to sleep that interferes with daily activities.
- Disrupted Sleep Cycle: A general feeling of un-restored sleep, regardless of the hours spent, leading to poor sleep quality and perpetuating fatigue.
Both too little and too much sleep can exacerbate depressive feelings and disrupt daily routines, creating a vicious cycle.
Changes in Appetite and Weight
Another significant physical change is a shift in eating habits, which can lead to noticeable weight fluctuations. Some individuals with depression symptoms experience a significant loss of appetite, leading to unintentional weight loss. Food may seem unappealing, or the effort to prepare and eat meals feels overwhelming. Conversely, others may experience an increase in appetite, often craving comfort foods, leading to weight gain. These changes can be dramatic and rapid, signaling an underlying mood disorder and should not be ignored.
Fatigue and Loss of Energy (Anergia)
A pervasive feeling of tiredness, even after adequate sleep, is a classic sign of depression. People with depression often describe feeling constantly drained, lacking the energy to perform even simple tasks. This extreme fatigue (anergia) isn’t relieved by rest and can make daily responsibilities, social interactions, and self-care feel like monumental efforts. It’s a profound lack of physical and mental energy that interferes with nearly all activities.
Aches, Pains, and Digestive Problems Without Clear Cause
Depression can manifest as unexplained physical symptoms, often referred to as somatic symptoms. These can include chronic headaches, back pain, muscle aches, digestive issues (like constipation or diarrhea), and generalized body aches, often without a clear medical cause. The mind-body connection is powerful, and mental distress can translate into real physical discomfort. Doctors might rule out other medical conditions before considering these as depression symptoms, highlighting the importance of a comprehensive medical evaluation.
Psychomotor Agitation or Retardation
These are more observable behavioral symptoms of depression, representing changes in a person’s physical activity and energy levels:
- Psychomotor Agitation: Restlessness, pacing, hand-wringing, an inability to sit still, or feeling keyed up and unable to relax. This can appear as nervous energy or constant fidgeting.
- Psychomotor Retardation: Slowed movements, speech, and thought processes; a noticeable decrease in physical activity and reaction time. This might manifest as delayed responses, speaking in a monotone, or moving as if in slow motion.
Both extremes indicate significant psychological distress and are often noticeable to those around the individual, serving as important signs of depression.
Recognizing the Red Flags: When to Seek Professional Help for Depression Symptoms
Identifying depression symptoms in yourself or a loved one is a crucial first step, but knowing when to transition from observation to action is equally important. Depression is a highly treatable condition, and early intervention can significantly improve outcomes and prevent further suffering. Here’s how to recognize the red flags that signal it’s time to seek professional help for symptoms of depression.
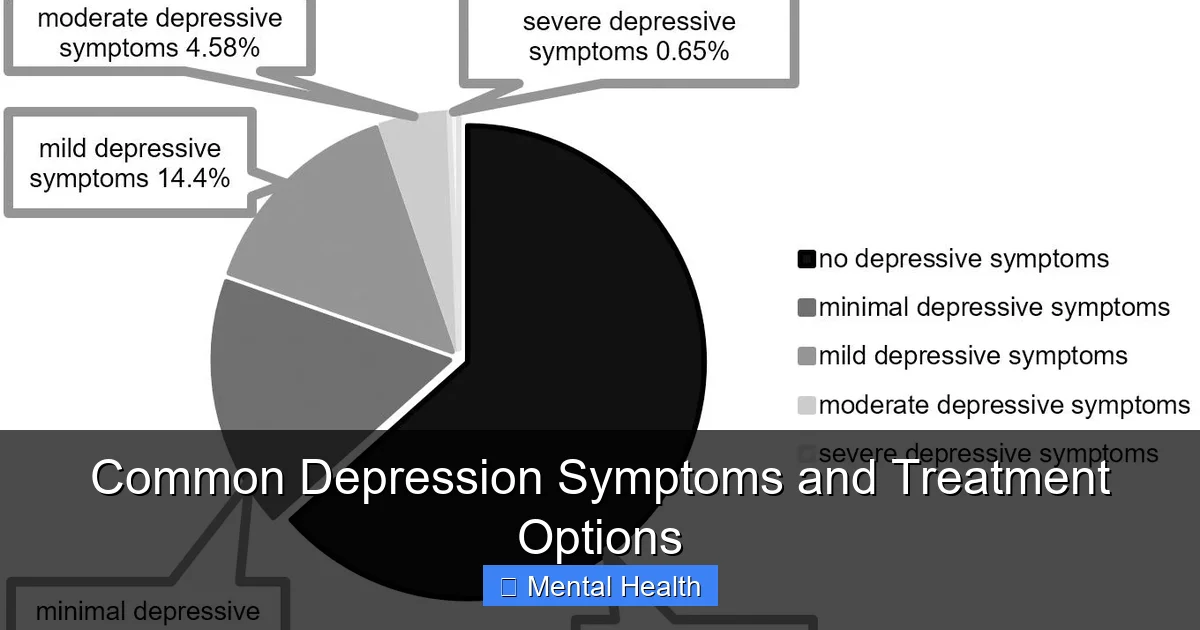
Duration and Severity of Symptoms
If you’ve been experiencing several of the aforementioned symptoms of depression for most of the day, nearly every day, for at least two consecutive weeks, it’s a strong indicator that professional assessment is needed. The severity matters too: are the symptoms mild and manageable, or are they significantly impairing your ability to function at work, school, or in relationships?
- Mild Depression: Symptoms are distressing but manageable, with minimal impact on daily life. You might still be able to maintain responsibilities, though with difficulty.
- Moderate Depression: Symptoms are more pronounced, causing noticeable difficulty in daily functioning and significant distress. Social and occupational impairment becomes more evident.
- Severe Depression: Symptoms are overwhelming, making it nearly impossible to function in daily life, often accompanied by strong feelings of worthlessness, hopelessness, or thoughts of self-harm or suicide. This level requires urgent attention.
Impact on Daily Life and Relationships
Consider how these depression symptoms are affecting your life. Are you withdrawing from friends and family, isolating yourself from social activities you once enjoyed? Are your grades or work performance suffering, leading to missed deadlines or decreased productivity? Is your personal hygiene declining, or are you struggling to maintain basic self-care? When depression begins to significantly disrupt your normal routines, relationships, and responsibilities, it’s a clear signal to seek help. The erosion of daily functioning is a powerful indicator that professional support is needed to address your mental health.
Self-Harm or Suicidal Thoughts
As mentioned earlier, any thoughts of self-harm, death, or suicide are absolute red flags that require immediate professional intervention. These thoughts are not normal and signify a severe level of distress. Do not try to manage these thoughts alone. Reach out to a mental health professional, emergency services, or a crisis hotline immediately. In the US, you can call or text 988 anytime. Your life is valuable, and help is available. Talking about these feelings can be the first step to finding relief and a path to safety.
Difficulty Coping and Feeling Overwhelmed
If you feel constantly overwhelmed by life’s demands, unable to cope with daily stressors, or if your usual coping mechanisms are no longer working effectively, it’s time to reach out. Mental health professionals can provide objective perspectives, new strategies, supportive guidance, and effective treatment plans to help you regain control and build resilience against depression symptoms. A persistent feeling of being unable to manage is a significant indicator that external support is beneficial.
Navigating the Path to Recovery: Effective Treatment Options for Depression
The good news about depression symptoms is that they are highly treatable. A combination of therapies, medication, and lifestyle adjustments often leads to significant improvement, allowing individuals to lead full and meaningful lives. The key is finding a treatment plan tailored to your specific needs, engaging actively with it, and understanding that recovery is a process, not a destination. No single approach works for everyone, so flexibility and open communication with your healthcare provider are essential.
Psychotherapy (Talk Therapy)
Psychotherapy is one of the most effective and widely recommended treatments for depression. It involves talking to a trained mental health professional (such as a psychologist, psychiatrist, or licensed therapist) in a confidential setting to identify and address the root causes of depression, develop healthy coping strategies, and change negative thought patterns. Common types include:
- Cognitive Behavioral Therapy (CBT): A highly effective therapy that focuses on identifying and changing distorted thinking patterns and problematic behaviors that contribute to and maintain depression. It teaches practical skills for managing depression symptoms.
- Interpersonal Therapy (IPT): Focuses on improving problematic relationships and social interactions that may be contributing to or exacerbated by depression. It helps individuals navigate grief, role disputes, role transitions, and interpersonal deficits.
- Psychodynamic Therapy: Explores how past experiences, unconscious conflicts, and early life relationships influence current feelings, behaviors, and mental health challenges. It aims to increase self-awareness and resolve underlying issues.
Therapy provides a safe space to process emotions, gain insights, and learn valuable tools for long-term mental well-being and resilience against depression symptoms.
Medication (Antidepressants)
For moderate to severe symptoms of depression, antidepressant medications may be prescribed, often in conjunction with psychotherapy. These medications work by balancing brain chemicals (neurotransmitters) that affect mood, sleep, appetite, and energy. Common types include Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), and atypical antidepressants, among others.
It’s crucial to understand:
- Antidepressants are not a “cure” but can significantly alleviate depression symptoms by correcting chemical imbalances.
- They often take several weeks (typically 2-4 weeks or more) to become fully effective, and initial side effects may occur before benefits are felt.
- Finding the right medication and dosage can involve some trial and error, requiring patience and close collaboration with your doctor.
- They should always be taken under the supervision of a medical doctor or psychiatrist, who can monitor effectiveness and manage potential side effects.
- Antidepressants are generally most effective when combined with psychotherapy, as therapy provides coping skills that medication alone cannot.
Lifestyle Adjustments and Complementary Approaches
While not a substitute for professional treatment, lifestyle changes can play a powerful supporting role in managing depression symptoms and improving overall well-being:
- Regular Exercise: Engaging in physical activity consistently (even moderate intensity) has been shown to boost mood, reduce stress hormones, and improve sleep quality. Exercise releases endorphins, natural mood lifters.
- Balanced Diet: Eating nutritious, whole foods can improve overall energy, cognitive function, and mood. Conversely, excessive sugar, processed foods, and unhealthy fats can negatively impact mental health.
- Adequate Sleep Hygiene: Establishing a consistent sleep schedule, creating a dark and quiet sleep environment, and avoiding screens before bedtime can significantly improve sleep quality.
- Mindfulness and Meditation: Practices that cultivate present-moment awareness can help reduce stress, improve focus, and promote emotional regulation, offering a sense of calm amidst distressing depression symptoms.
- Social Connection: Reaching out to supportive friends and family, or joining support groups, can combat feelings of isolation and provide a sense of belonging. Even small social interactions can make a difference.
- Limit Alcohol and Drugs: While they might offer temporary relief, these substances can worsen depression over time, interfere with medication, and disrupt healthy coping mechanisms.
- Engage in Hobbies: Re-engaging with activities you once enjoyed, even if it feels difficult at first, can gradually restore a sense of pleasure and purpose.
Living Well with Depression: Long-Term Management and Support
Managing depression symptoms is often an ongoing journey, not a one-time fix. Even after initial treatment, maintaining mental well-being requires continuous effort and a robust support system. Developing long-term strategies is key to preventing relapse and fostering a fulfilling life, allowing you to not just survive but thrive despite the challenges of depression.
Building a Strong Support System
One of the most vital components of long-term management is having a reliable support network. This can include family, friends, support groups (online or in-person), or a trusted therapist. Knowing you have people to talk to, who understand or are willing to learn about your symptoms of depression, can provide immense comfort and practical help. Don’t be afraid to lean on others and communicate your needs openly; vulnerability can foster deeper connections and reduce the burden you carry.
Developing Healthy Coping Strategies
Working with a therapist can help you identify and develop healthy, adaptive coping mechanisms to navigate stressful situations and potential triggers for your depression symptoms. These might include:
- Journaling to process emotions and gain perspective on your thoughts.
- Practicing relaxation techniques like deep breathing exercises, progressive muscle relaxation, or yoga to calm your nervous system.
- Engaging in creative outlets such as art, music, or writing as a form of self-expression and emotional release.
- Setting realistic, achievable goals and celebrating small victories to build a sense of accomplishment and self-efficacy.
- Learning to say “no” and setting healthy boundaries to protect your energy and prevent burnout.
- Developing problem-solving skills to address life challenges proactively rather than being overwhelmed by them.
Monitoring and Relapse Prevention
Understanding your personal triggers and early warning signs is crucial for preventing a full-blown depressive episode. Keep track of your mood, energy levels, sleep patterns, appetite, and any return of common depression symptoms. This self-monitoring can be done through a journal or a mood tracking app. If you notice signs of a relapse, contact your healthcare provider promptly. Having a relapse prevention plan in place, developed with your therapist, can be incredibly empowering and provide a clear course of action when you need it most.
The Importance of Ongoing Care
Even when you feel better, continuing with regular therapy sessions (even if less frequent) or medication management (if prescribed) can be essential. Depression is a chronic condition for many, and ongoing care helps maintain stability and addresses any emerging challenges. Regular check-ins with your doctor or therapist ensure your treatment plan remains effective and can be adjusted as needed. Proactive maintenance is far easier than reactive crisis management when dealing with mental health challenges.
Relevant Depression Statistics (Data Table)
Understanding the widespread impact of depression can help contextualize its severity and underscore the importance of seeking help for depression symptoms. These statistics highlight the global burden and the need for continued awareness and support.
| Statistic | Source | Details |
|---|---|---|
| Global Prevalence of Depression | WHO (World Health Organization) | Over 280 million people worldwide suffer from depression, making it a significant global health challenge. |
| Leading Cause of Disability | WHO | Depression is one of the leading causes of disability worldwide, contributing substantially to the global burden of disease. |
| Youth Depression in the U.S. | NIH / SAMHSA (2022) | Approximately 17% of U.S. youth (ages 12-17) experienced a major depressive episode in the past year, indicating a rising trend among adolescents. |
| Adult Depression in the U.S. | NIH / SAMHSA (2022) | Around 8.3% of all U.S. adults (21 million) experienced at least one major depressive episode in the past year, underscoring its widespread impact on the adult population. |
| Treatment Gap | Various Studies (e.g., Lancet Psychiatry) | Globally, over 75% of people in low- and middle-income countries receive no treatment for depression. Significant gaps also exist in high-income countries, highlighting barriers to access and stigma. |
These figures highlight the pervasive nature of depression and the critical need for increased awareness, destigmatization, and access to effective treatment for depression symptoms across all demographics.
Conclusion: Taking the First Step Towards Hope and Healing
Recognizing the common depression symptoms is a powerful act of self-awareness and compassion, whether for yourself or a loved one. Depression is a serious, yet highly treatable, mental health condition that impacts millions globally, manifesting in a diverse range of emotional, physical, and behavioral signs. From persistent sadness and a profound loss of pleasure to significant changes in sleep, appetite, and energy, the myriad ways symptoms of depression can present themselves underscore the complexity of this disorder. It’s a pervasive illness that demands our attention, understanding, and proactive response.
Remember, you don’t have to navigate this journey alone. Understanding the signs of depression empowers you to seek timely professional help, which is crucial for recovery. With effective treatment options like psychotherapy, medication, and supportive lifestyle changes, individuals can significantly alleviate their depression symptoms and reclaim their lives. The path to healing begins with acknowledging the problem and reaching out. Take that brave first step—it could be the most important one you ever make for your mental health. Support is available, and recovery is possible. Your well-being matters, and there is always hope for a brighter, more fulfilling future.
Frequently Asked Questions
What are the most common depression symptoms?
Depression symptoms often include persistent feelings of sadness, loss of interest or pleasure in activities you once enjoyed, and significant changes in appetite or sleep patterns. You might also experience fatigue, feelings of worthlessness or guilt, and difficulty concentrating or making decisions.
Can depression symptoms manifest as physical pain or discomfort?
Yes, depression symptoms can absolutely include various physical aches and pains without a clear medical cause. These might present as chronic headaches, digestive problems, back pain, or general body aches that don’t respond to typical treatments.
How long do depression symptoms typically last before professional help is recommended?
If depression symptoms persist for most of the day, nearly every day, for two weeks or longer, it’s generally recommended to seek professional help. Untreated symptoms can worsen over time and significantly impact your quality of life.
Are there different depression symptoms for men compared to women?
While many core depression symptoms are universal, men sometimes exhibit irritability, anger, or escapist behavior like substance abuse, rather than overt sadness. Women, on the other hand, may be more prone to feelings of guilt, worthlessness, and atypical symptoms like increased appetite or hypersomnia.
What’s the difference between normal sadness and clinical depression symptoms?
Normal sadness is a temporary emotional response to life events, often lessening over time. Clinical depression symptoms are more severe, pervasive, and persistent, significantly impairing daily functioning and often occurring without an obvious trigger, lasting for weeks or months.
When should I seek professional help for depression symptoms?
You should seek professional help for depression symptoms if they are significantly impacting your daily life, causing distress, or if you are having thoughts of self-harm or suicide. A doctor or mental health professional can provide an accurate diagnosis and discuss appropriate treatment options.